Clinical history
The patient is an 81 year old male with no significant past medical history who presented with abdominal pain, nausea and weight loss of several months duration.
Labs
ALT 15 U/L, AST 55 U/L, ALK PHOS 81 U/L, total bilirubin 0.3 mg/dl. Tumor makers: AFP 1 IU/ml, CEA 2.4 ng/ml CA19-9 55 U/ml, PSA 11.35 ng/ml.
Radiology
CT scan showed four liver masses which measured up to 3.6 cm, a 6.9 cm left kidney mass and an 8.9 cm mesenteric mass. A CT-guided biopsy of the liver mass was performed.
Microscopic images
 |
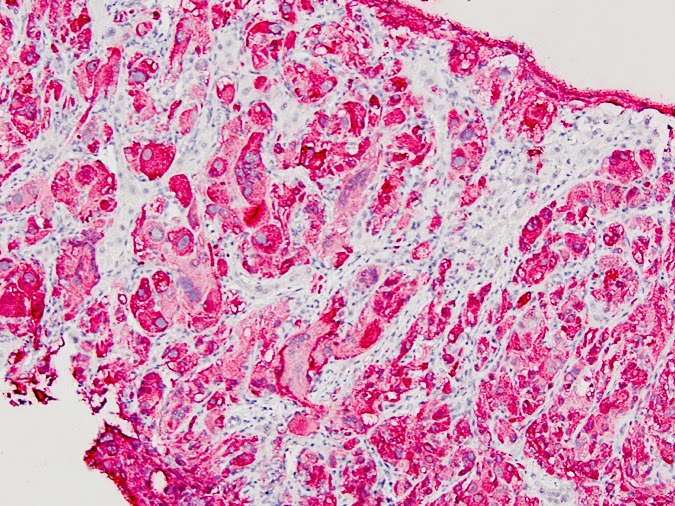
| Figure 1 |
 |
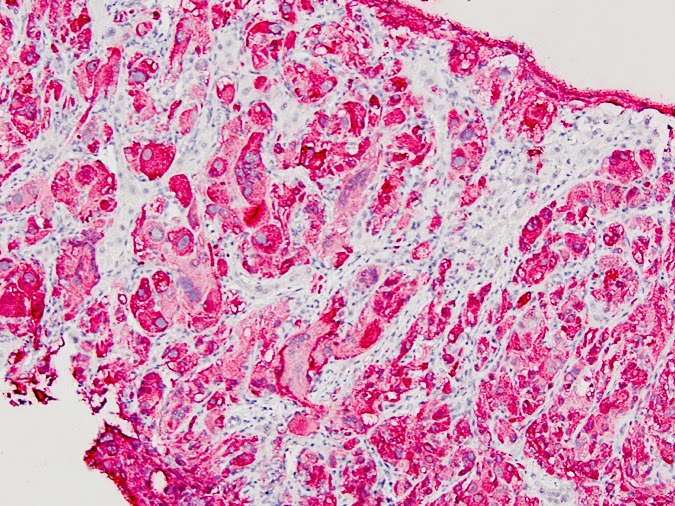
| Figure 2 |
 |
| Figure 3 |
 |
| Figure 4 |
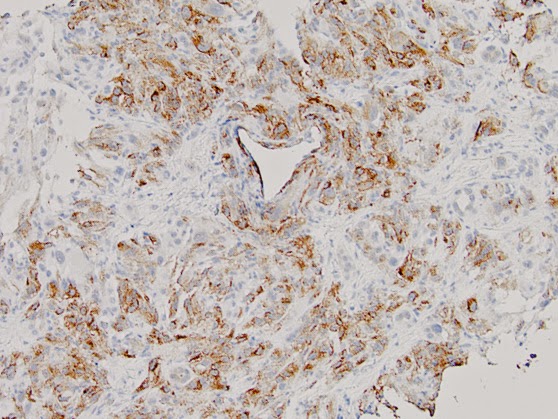 |
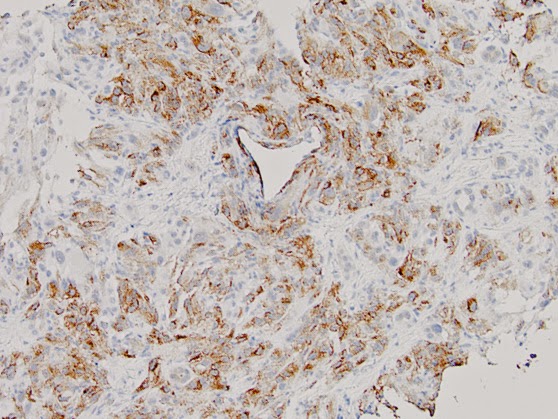
| Figure 5, HMB-45 |
 |
| Figure 6, Melan A |
 |
| Figure 7, CD10 |
 |
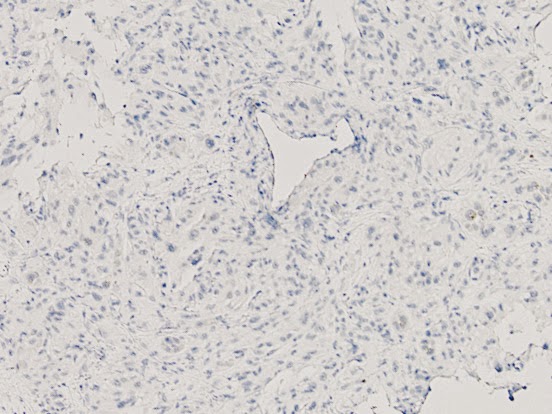
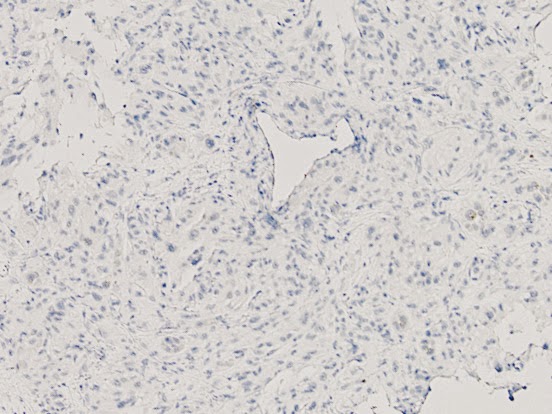
| Figure 8, AE1/AE3 |
 |
| Figure 9, S-100 |
Diagnosis
Metastatic malignant epithelioid angiomyolipoma.
Discussion
This tumor demonstrates a proliferation of predominantly large epithelioid cells with abundant eosinophilic cytoplasm, vesicular nuclei, and prominent nucleoli (Figure 1). Focal tumor cell spindling is seen (Figure 2). Scattered ganglion-like cells and multinucleated giant cells are present (Figure 3). Mitoses, including atypical mitotic figures, are present (Figure 3 and Figure 4). No necrosis is identified. The tumor cells are positive by immunohistochemistry (IHC) for HMB45 (Figure 5), Melan A (Figure 6), CD10 (Figure 7), MiTF, and CD68; they are negative for cytokeratin AE1/AE3 (Figure 8), S100 (Figure 9), CAM 5.2, CD117, CD34, SMA, desmin, calponin, myogenin, and inhibin.
The differential diagnosis includes, but is not limited to, renal cell carcinoma with sarcomatoid differentiation, adrenal cortical carcinoma, melanoma, malignant GIST, undifferentiated/sarcomatoid carcinoma and malignant epithelioid angiomyolipoma. Combined epithelioid and spindle cell morphology, large ganglion-like cells and multinucleated giant cells are characteristic of epithelioid angiomyolipoma (E-AML). Positive IHC for HMB45, Melan A, MiTF and CD68, together with negative IHC for epithelial markers and S100 help confirm the diagnosis. However, as we are always taught, “melanoma is the great mimicker” and rarely melanoma can be S-100 negative.
The usual renal angiomyolipoma (AML) is considered a benign mesenchymal tumor composed of a variable portion of fat, smooth muscle cells, and abnormal thick-walled vessels. E-AML is a rare variant and potentially malignant neoplasm composed partially or entirely of epithelioid cells. Up to one-third of E-AML patients experience local recurrences and/or distant metastases. Features that favor malignant E-AML include nuclear atypical in ≥70% of the epithelioid cells, ≥2 mitotic figures per 10 high power fields, atypical mitotic figures, and necrosis; the presence of 3 or all of these features is predictive of aggressive behavior (Brimo F, Robinson B, Guo C et al. Am J Surg Pathol 2010;34:715-722). E-AMLs are immunoreactive for one or more melanocytic markers (e.g., HMB45, Melan A, and MiTF). They often express smooth muscle markers such as SMA and desmin. The absence of S100 staining can help distinguish E-AML from melanoma. The absence of staining for epithelial markers can help distinguish E-AML from carcinoma.
Patient follow up:
Shortly after the diagnosis of malignant E-AML was made in August of 2013, the patient was started on Afinitor 10 mg daily (also called everolimus, an established medication for AML). He had an excellent initial response (CT scan in early 2014 showed significantly reduced size of the mesenteric mass with stable liver and kidney masses). However, the treatment was held several times due to severe side effects including hyponatremia, diarrhea and fevers. Afinitor was re-started in July of 2014 at a very low dose. Currently, one year since diagnosis, the patient is doing reasonable well with no new masses.
Contributed by
Wendy Cao, MD