Interesting Case May 2014
Clinical History
This 23 year old woman is status post allogeneic BMT for Fanconi anemia 15 years prior. She was generally doing well, but was lost to follow up at our institution since 5 years ago. She presented to an outside pediatrician with complaint of fatigue, malaise, abdominal pain and pruritus for the past couple of months.
Labs
At the time of presentation her alkaline phosphatase >700 U/L, AST 100-200 U/L, ALT 200-300 U/L and total bilirubin 18-20 mg/dL.
Microscopic Images
 |
| Figure 1 |
 |
| Figure 2 |
 |
| Figure 3 |
 |
| Figure 4 |
 |
| Figure 5 |
 |
| Figure 6 |
Diagnosis
Chronic graft versus host disease
Discussion
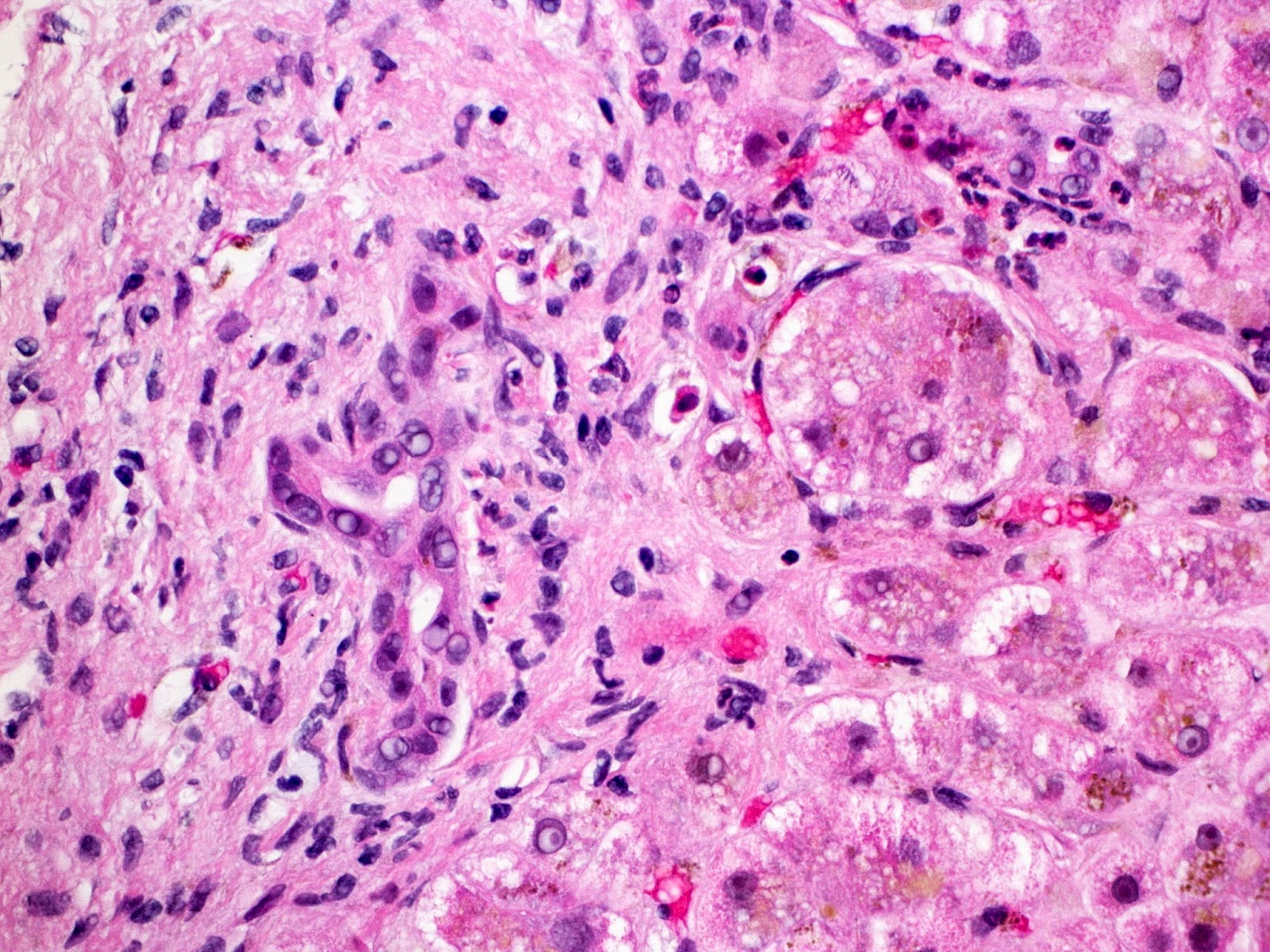
Figure 1 shows a large portal area with several vascular profiles and lack of interlobular bile duct. Figure 2 shows the only bile duct identified on multiple levels. This duct shows features of injury including loss of nuclear polarity and nuclear hyperchromasia.
Figure 3 shows marked canalicular cholestasis.
Figure 4 is the keratin 19 stain confirming a lack of interlobular bile duct and essentially no ductular reaction.
Figures 5 and 6 show portal-portal bridging fibrosis at least.
The paucity of interlobular bile ducts and lack of ductular reaction raises several possibilities. The top of the list in this setting would be chronic graft versus host disease (GVHD). However, advanced fibrosis with chronic GVHD is rarely described. From the available clinical records, this patient has a history of chronic skin and liver GVHD that has responded well to immunosuppression in the past. Furthermore, the patient intermittently electively takes herself off immunosuppressive therapy with resultant flares, as happened in this case.
The differential diagnosis would also include drug/medication induced “vanishing bile duct syndrome”. The lack of a history of drug induced cholestatic hepatitis, the presence of what appears to be well documented chronic cutaneous GVHD, along with prompt symptomatic and laboratory improvement with reestablishment of immunosuppression support chronic liver GVHD. In this age group, the differential diagnosis would also include primary sclerosing cholangitis. Although no cholangiogram was performed, the patient underwent abdominal MRI with and without contrast which showed no evidence of intra- or extrahepatic biliary ductal dilation and she has no history of inflammatory bowel disease.
As the outcomes for BMT patients continue to improve and the duration of patient survival is extended, perhaps we will see more cases of chronic GVHD with advanced fibrosis.
Contributed by
Cynthia D. Guy, MD
